By DR. Richard Bosshardt
Miracle weight loss drug or dangerous new fad?

I recently became aware of a new darling in the never-ending search for a magic bullet to weight loss. Semiglutide (brand names Ozempic and Wegovy) is an oral or injectable drug in a class of drugs called glucagon-like protein 1 (GLP-1) receptor antagonists used to treat type II diabetes, the type usually associated with being overweight or obese.
In simple terms, two hormones control blood sugar levels – glucagon and insulin. Glucagon raises blood sugar, and insulin lowers it. GLP-1 receptor antagonists like Ozempic work to lower blood sugar. They also have a large number of other potential and known actions. They may be neuroprotective (reducing inflammation of nerves), may lower blood pressure, and may reduce liver inflammation. One of their most interesting effects is on brown fat, which makes up a small percentage of the fat in your body (as opposed to white fat) but is more metabolically active. Brown fat helps regulate body temperature and stabilizes blood sugar. Ozempic activates brown fat.
Approved by the FDA in December 2017 for treatment of type II diabetes, Ozempic was subsequently noted to suppress appetite and reduce weight in users. Recently, its popularity has exploded amid speculation about newly thin celebrities and influencers who seem to have lost weight almost overnight. Although only FDA-approved for diabetes and available only by prescription, off-label use of Ozempic has skyrocketed for weight loss. And it is easily obtained by anyone who wants it and can afford the hefty price tag of around $1,000 for a multi-dose pen that lasts one month.
Ozempic is offered at medical spas that have a “medical director” who is a physician or dentist who can prescribe medications. Finding prescribers for a med spa is easy. Many are retired physicians looking for the extra income or just something to do. Most have no direct involvement with the spa clients. Often, no office visit is required for an Ozempic script.
In 24 states, nurse practitioners (NP) also have full and unrestricted prescribing privileges. Florida is a restricted privilege state and NPs must be under supervision of a physician.
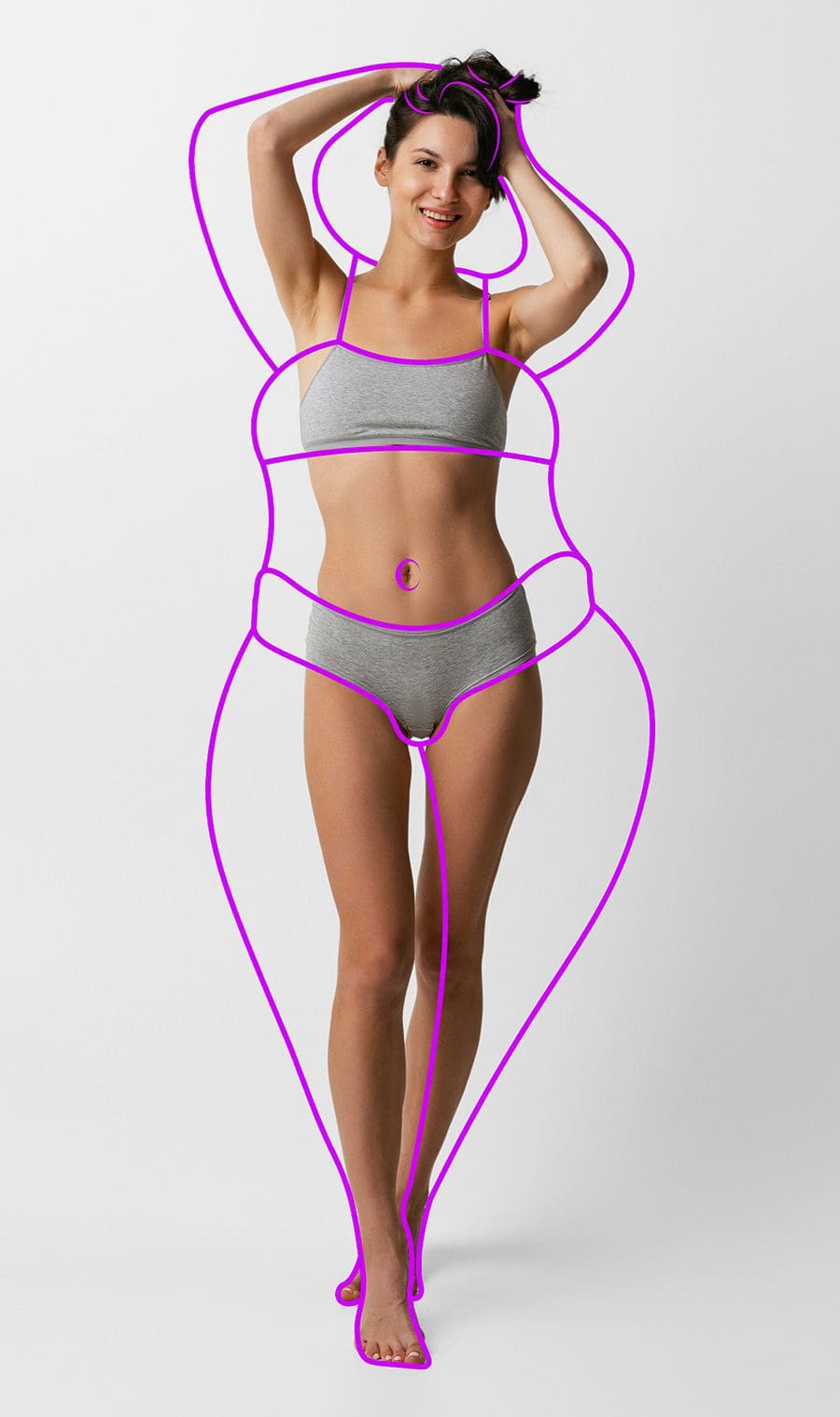
The demand for Ozempic is understandable. No one disputes that we’re dealing with an obesity epidemic. Forty percent of the U.S. population is obese (a body mass index of 30 or above**). What does that look like? This: a 5’ 6” woman weighing more than 186 lbs. and/or a 5’ 11” man weighing more than 215 lbs. Both are obese.

Thirty-eight percent of the U.S. population is overweight, defined as a body mass index of 26 or more. One of the most worrisome aspects of the obesity epidemic is that 20 percent of children age 2-19 are obese (defined as weighing at or more than 95 percent of their peers). And childhood obesity sets a person up for a lifetime of battling their weight.
Why does weight matter? Despite the social and cultural controversy regarding body positivity and fat-shaming, it is a simple medical fact that there are serious health consequences to being overweight . . . and these increase greatly with obesity. High blood pressure, type II diabetes, heart disease, fatty liver disease, and osteoarthritis are related to weight. Cancers, such as breast and colon cancer, are more common in those with unhealthy weight.
And obesity is one of the most significant risk factors for serious illness due to COVID-19 and other infectious illnesses. Also, being overweight or obese increases the risk of complications from surgery.

In the U.S. today, it’s difficult to calculate, much less comprehend, the health costs of being overweight or obese and how much money is spent on treatment, as well as medical problems associated with carrying excess weight. In 2013, $170 billion dollars was spent treating obesity and related problems, or 16 percent of health care dollars. Combined with an aging population and poor lifestyle habits, it is no exaggeration to state that health care costs pose an existential threat to the future of the U.S. economy. If that threat materializes, obesity will lead the charge.
Into this unsustainable situation enters Ozempic, an injectable medication anyone can learn to self-administer once a week. Voila! Pounds drop off, seemingly without effort. No diet or exercise required. What could be simpler?
Medicine and the human body are never simple and most efforts to offer simple solutions to complex problems, such as obesity, almost always are bound to fail.
All weight loss is not equal. Anyone can lose weight simply by not eating. You do not see obese people in countries where the population is starving. Starvation causes loss of fat. Starvation also causes lean body mass, which is everything that is not fat – primarily muscle, bones, tendons, and ligaments. Loss of lean mass can be unhealthy in several ways.
In the U.S. we have a unique situation – most of our poor are overweight or obese. Starvation causes loss of both fat and lean body mass. The latter is everything that is not fat – muscle, bones, tendons, ligaments, and such. Loss of lean mass can be unhealthy in several ways.
Lean body mass is more metabolically active, i.e. burns more calories, and helps control weight. It fights insulin resistance, a hallmark of type II diabetes. It keeps bones strong, which is especially important in post-menopausal women, many who have reduced bone strength. It makes us more physically capable, giving us strength to avoid falls and to get up when we do fall (emergency rooms regularly see elderly patients who have fallen and do not have the strength to get up.)
The goal of healthy weight loss is not merely to lose fat. The goal should be to improve body composition – the ratio between fat and lean body mass. A healthy ratio of fat to lean body mass is around 30 percent or less in adult women, and 25 percent or less in adult men.
In healthy weight loss, lean body mass makes up about 25 percent of the lost weight. This can be reduced by eating more protein and exercising, especially weight and resistance training, both which build muscle.
In studies of Ozempic, the percentage of lean body mass lost to fat is 40 percent. This can become significant in older, obese individuals who already have less lean body mass than ideal. It can also become an issue in people who are not truly overweight or obese but are using Ozempic in hopes of achieving some ideal weight goal.
In addition to the unacceptably high ratio of lean body mass loss, Ozempic use has other problems. First, some people experience side effects of nausea, vomiting, and diarrhea. The specter of cancer, e.g. thyroid cancer, has been raised in some early studies on rats. Finally, most people report putting the weight back on after discontinuing the shots. And the high cost means that few people will stay on Ozempic for very long.
I doubt Ozempic will supplant tried and true ways of losing weight – a healthy diet, regular exercise, and a generally healthy lifestyle. I predict that sometime in the not-too-distant future we will be asking, “Whatever happened to Ozempic?”
**A professional athlete, such as a football player, may have a BMI in the obese range but minimal body fat, as most of the weight is lean muscle and bone.